 Cholesterol screening guidelines provide a more personalized approach to determining who needs testing and when. They better identify individuals requiring earlier or extra monitoring based on risk profiles.
Cholesterol screening guidelines provide a more personalized approach to determining who needs testing and when. They better identify individuals requiring earlier or extra monitoring based on risk profiles.
Understanding the latest recommendations allows you to take more informed control of safeguarding your long-term heart health.
What Cholesterol Is and Why Undergo Screening
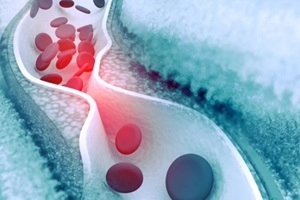
Cholesterol represents a soft, waxy substance your body utilizes to function properly. The liver produces all the cholesterol you need naturally. However, overconsuming foods high in saturated fats prompts the liver to overproduce cholesterol unnecessarily.
When higher amounts circulate in the bloodstream than optimal over longer periods, it gradually accumulates inside artery walls as plaque buildup. This atherosclerotic process hardens and narrows blood vessels, impairing blood flow. It dramatically escalates the likelihood of eventually facing a debilitating heart attack or stroke.
Screening involves obtaining a lipoprotein blood test that measures healthy HDL cholesterol, LDL cholesterol, total cholesterol levels, and triglyceride values. Maintaining your cholesterol numbers within the following healthy ranges reduces the chances of atherosclerosis down the road:
- Total cholesterol: <170 mg/dL
- LDL “bad” cholesterol: <100 mg/dL
- HDL “good” cholesterol: ≥40 mg/dL men / ≥50 mg/dL women
- Triglycerides: <150 mg/dL
What’s in the Cholesterol Screening Guidelines
Rather than endorse a universal cholesterol testing schedule for all adults, as was previously the case, current guidelines focus more closely on pinpointing specific people needing earlier intervention or more frequent monitoring by assessing individual risk factor profiles. They customize screening timing/frequency and cholesterol targets based on careful evaluation of the following:
 Personal health metrics such as blood pressure, blood sugar, and weight
Personal health metrics such as blood pressure, blood sugar, and weight- Medication needs and adherence patterns
- Tobacco usage habits
- Age, gender, and family histories of early cardiovascular disease
- Baseline cholesterol levels and response to lifestyle changes
- The presence of related health conditions such as diabetes and chronic kidney disease
Leveraging this deeper analysis of distinctive risk parameters allows vastly more personalized programs catered to an individual’s unique situation instead of blanket recommendations.
After thoroughly reviewing risk profiles, providers calculate 10-year risk percentages for experiencing heart attack, stroke, and related atherosclerotic cardiovascular disease (ASCVD) events.
They then dial in cholesterol targets proportional to estimated ASCVD risk. The highest-risk cohort now sees aggressive LDL goals below 70 mg/dL spurred by promptly starting a medication regimen plus lifestyle improvements, while lower-risk groups adopt more moderate, personalized cholesterol targets.
Preparing to Discuss Your Situation
Next time bloodwork gets ordered, request adding on a lipoprotein profile if you lack recent cholesterol values to establish a baseline for tracking purposes. Then, arrive at your visit equipped to have an open, productive conversation about what makes sense moving forward in your case.
Consider asking questions such as:
- Based on my health stats and family history, should I undergo routine cholesterol screening going forward? How often do you recommend?
- What are my latest total cholesterol, LDL, HDL, and triglycerides levels?
- What do my present cholesterol numbers suggest about both my current and long-term heart disease risks? Should I take preventative action?
- Do my results fall within or outside the ideal recommended ranges? By how much do they differ if not optimal?
- Can you outline specific nutrition and lifestyle changes to help optimize my cholesterol and reduce cardiovascular risks?
- Will initiating or intensifying cholesterol medication be warranted in my situation?
Discussing personal risk parameters and screening findings makes determining appropriate next steps more straightforward. It facilitates tailored lifestyle, monitoring, and treatment plans to strengthen lifelong cardiovascular health proactively.
Expanding Approaches to Cholesterol Medication
The guidelines highlight using risk-aligned, personalized thresholds for starting cholesterol medication instead of a blanket one-size-fits-all strategy.
They also advise considering non-statin agents such as PCSK9 inhibitors – alone and combined with statins – in high-risk patients unable to reach their LDL targets through maximized statin doses paired with lifestyle adjustments alone.
Statins remain the first choice when it comes to cholesterol treatments for most people needing medication since they are affordable and effective while posing minimal side effects for a majority of patients.
However, relatively newly developed medications, such as PCSK9 inhibitors, when combined with statins, can further lower LDL by up to 60%, even in individuals not responding sufficiently to other therapies.
Lifestyle and Age Affect Risk Too
 Atherosclerosis builds slowly over many years, meaning establishing healthy long-term patterns early on—such as optimal nutrition, regular exercise, and avoiding tobacco—pays dividends by substantially cutting your lifetime cardiovascular risks.
Atherosclerosis builds slowly over many years, meaning establishing healthy long-term patterns early on—such as optimal nutrition, regular exercise, and avoiding tobacco—pays dividends by substantially cutting your lifetime cardiovascular risks.
As a result, the guidelines suggest considering baseline cholesterol screening for more adults under 40 without other risk factors.
This way, potential issues get uncovered right away before causing permanent damage. Catching them early means lifestyle improvements have the best shot at making an impact.
Finding and controlling borderline cholesterol levels sooner rather than later significantly reduces plaque accumulation inside arteries over the long run. This dramatically lowers the odds of eventually developing heart disease.
Turn to Imperial Center Family Medicine for Your Cholesterol Screening
Cholesterol screening guidelines recommend personalized screening based on your risk profile. However, recommendations change based on age and particular situations, which can be confusing.
Imperial Center Family Medicine is here to help. Our expert healthcare professionals stay current on evidence-based protocols so we can best advise patients on appropriate testing timing.
If you have any uncertainty about your cholesterol levels, recommended testing frequency, or risk factors needing attention, contact us today at 919-873-4437 or online to schedule an appointment.